THE BACK PAGE
WHAT IS BACK PAIN?
BACK PAIN is a term that is used to refer to a whole host of back related issues, from the relatively minor muscular pain to to full blown excrutiatingly severe prolapsed disc pain that can result in
the loss of muscular control.
The former can be treated quite easily with localised ointments, lotions, and weak analgesics. However, it is the latter that will be discussed in detail.
As a common neurological ailment, back pain affects both Men and women equally. It occurs most often between ages 30 and 50, due in part to the aging process but also as a result of sedentary life
style, and is a common cause of job-related disability
and missed work. Most occurrences of lower back pain go away within a few days. Others take much longer to resolve or lead to more serious conditions.
Acute back pain generally lasts from a few days to a few weeks. Most acute back pain is mechanical in nature, the result of trauma to the lower back or a disorder such as arthritis.
There are a variety of causes of lower back pain from trauma, including sports related injuries, lifting inadequatley and unsafely, and other stressors o the
spine.
Symptoms may range from muscle ache to shooting or stabbing pain, limited flexibility and/or range of motion, or an inability to stand straight.
Pain felt in one part of the body may radiate from a problem elsewhere in the body.
Some acute pain syndromes can become more serious if left untreated.
Lower back pain unrelated to injury or other known cause is unusual in pre-teen children, although, heavy backpacks can strain the back.Chronic back pain is measured by duration, pain that persists
for more than 3 months is considered chronic. It is often progressive and the cause can be difficult to determine.
Risks of lower back pain from disc disease or spinal degeneration increase with age.There are a few specific types of severe back pain, or as my doctore describes it, "BACK ACHE"!!!
Two of the most severe types of lower back pain are closely related and can come in a various combinations. These are the herniated disc and the prolapsed disc.
I have compiled some information from a variety of sources from the internet for you so that you'll not need to searcg for everything yourself. I don't have everything here, but you'll get a better
idea. I've provided references at the end.
THE PROLAPSED DISC
A prolapsed disc often causes severe lower back pain. The disc often presses on a nerve root which also causes pain and other symptoms in a leg. In most cases, the symptoms ease off gradually over
several weeks. The usual advice is to do normal activities as much as possible. Painkillers may help. Physical treatments such as spinal manipulation may also help. Surgery may be an option if the
symptoms persist.
Understanding the back
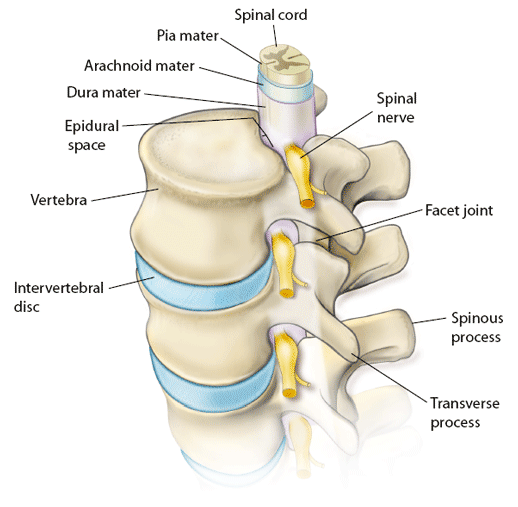
The spine is made up of many bones called vertebrae. These are roughly circular and between each vertebra is a 'disc'. The discs are made of strong 'rubber-like' tissue which allows the spine to be
fairly flexible. A disc has a stronger fibrous outer part, and a softer jelly-like middle part called the nucleus pulposus.
The spinal cord, which contains the nerves that come from the brain, is protected by the spine. Nerves from the spinal cord come out from between the vertebrae to take and receive messages to various
parts of the body.
Strong ligaments attach to the vertebrae. These give extra support and strength to the spine. Various muscles also surround, and are attached to, various parts of the spine. (The muscles and
ligaments are not shown in the diagram below for clarity.)
What is a prolapsed disc?
When you have a prolapsed disc (commonly called a 'slipped disc'), a disc does not actually 'slip'. What happens is that part of the inner softer part of the disc (the nucleus pulposus) bulges out
(herniates) through a weakness in the outer part of the disc. A prolapsed disc is sometimes called a herniated disc. The bulging disc may press on nearby structures such as a nerve coming from the
spinal cord. Some inflammation also develops around the prolapsed part of the disc.
Any disc in the spine can prolapse. However, most prolapsed discs occur in the lumbar part of the spine (lower back). The size of the prolapse can vary. As a rule, the larger the prolapse, the more
severe the symptoms are likely to be.
Who gets a prolapsed disc?
Bouts of back pain are very common. However, less than 1 in 20 cases of acute (sudden onset) back pain are due to a prolapsed disc. (Most cases on back pain are classed as 'simple low back pain'.
This is thought to be caused by a minor problem to a muscle, ligament, or other structure in the back. For example, a strained muscle. See separate leaflet called 'Low back Pain in Adults' for
a general overview of the different types of back pain.)
The commonest age to develop a prolapsed disc is between 30 and 50 years. Twice as many men as women are affected.
What causes a prolapsed disc?
It is not clear why some people develop a prolapsed disc and not others, even when they do the same job or lift the same sort of objects. It seems that some people may have a weakness in the outer
part of the affected disc. Various things may trigger the inner softer part of the disc to prolapse out through the weakened outer part of the disc. For example, sneezing, awkward bending, or heavy
lifting in an awkward position may cause some extra pressure on the disc. In people with a weakness in a disc this may be sufficient to cause a prolapse. Factors that may increase the risk of
developing a prolapsed disc include: a job involving lots of lifting, a job involving lots of sitting (especially driving), weight bearing sports (weight lifting, etc), smoking, obesity, and
increasing age (a disc is more likely to develop a weakness with increasing age).
What are the symptoms of a prolapsed disc?
Back pain
The pain is often severe, and usually comes on suddenly. The pain is usually eased by lying down flat, and is often made worse if you move your back, cough, or sneeze.
Nerve root pain (usually 'sciatica')
Nerve root pain is pain that occurs because a nerve coming from the spinal cord is pressed on ('trapped') by a prolapsed disc, or is irritated by the inflammation caused by the prolapsed disc.
Although the problem is in the back, you feel pain along the course of the nerve in addition to back pain. Therefore, you may feel pain down a leg to the calf or foot. Nerve root pain can range from
mild to severe, but it is often worse than the back pain. With a prolapsed disc, the sciatic nerve is the most commonly affected nerve. (The term 'sciatica' means nerve root pain of the sciatic
nerve.) The sciatic nerve is a large nerve that is made up from several smaller nerves that come out from the spinal cord in the lower back. It travels deep inside the buttock and down the back of
the leg. There is a sciatic nerve for each leg.
Other nerve root symptoms
The irritation or pressure on the nerve next to the spine may also cause pins and needles, numbness or weakness in part of a buttock, leg or foot. The exact site and type of symptoms depends in which
nerve is affected.
Cauda equina syndrome - rare, but an emergency
Cauda equina syndrome is a particularly serious type of nerve root problem that can be caused by a prolapsed disc. This is a rare disorder where the nerves at the very bottom of the spinal cord are
pressed on. This syndrome can cause low back pain plus: problems with bowel and bladder function (usually unable to pass urine), numbness in the 'saddle' area (around the anus), and weakness in one
or both legs. This syndrome needs urgent treatment to preserve the nerves to the bladder and bowel from becoming permanently damaged. See a doctor immediately if you develop these symptoms.
Some people do not have symptoms
Research studies where routine back scans have been done on a large number of people have shown that some people have a prolapsed disc without any symptoms. It is thought that symptoms mainly occur
if the prolapse causes pressure or irritation of a nerve. This does not happen in all cases. Some prolapses may be small, or occur away from the nerves and cause minor, or no symptoms.
How does a prolapsed disc progress?
In most cases, the symptoms tend to improve over a few weeks. Research studies of repeated MRI scans have shown that the bulging prolapsed portion of the disc tends to get smaller (regress) over time
in most cases. The symptoms then tend to ease, and go in many cases. In only about 1 in 10 cases is the pain still bad enough after six weeks to consider surgery (see below).
Do I need any tests?
Your doctor will normally be able to diagnose a prolapsed disc from the symptoms and by examining you. (It is the common cause of sudden back pain with nerve root symptoms.) In most cases, no tests
are needed as the symptoms often settle within a few weeks.
Tests such as x-rays or scans my be advised if symptoms persist. In particular, an MRI scan can show the site and size of a prolapsed disc. This information is needed if treatment with surgery is
being considered.
What are the treatments for a prolapsed disc?
Exercise and keep going
Continue with normal activities as far as possible. This may not be possible at first if the pain is very bad. However, move around as soon as possible, and get back into normal activities as soon as
you are able. As a rule, don't do anything that causes a lot of pain. However, you will have to accept some discomfort when you are trying to keep active. Setting a new goal each day may be a good
idea. For example, walking around the house on one day, a walk to the shops the next, etc.
In the past, advice had been to rest until the pain eases. It is now known that this was wrong. You are likely to recover more quickly and are less likely to develop chronic (persistent) back pain if
you keep active when you have back pain rather than rest a lot. Also, sleep in the most naturally comfortable position on whatever is the most comfortable surface. (Advice given in the past used to
be to sleep on a firm mattress. However, there is no evidence to say that a firm mattress is better than any other type of mattress for people with back pain.)
Medication
If you need painkillers, it is best to take them regularly. This is better than taking them 'now and again' just when the pain is very bad. If you take them regularly the pain is more likely to be
eased for much of the time and enable you to exercise and keep active.
- Paracetamol is often sufficient if you take it regularly at full strength. For an adult, this is 1000 mg (usually two 500 mg tablets), four times a day.
- Anti-inflammatory painkillers. Some people find that these work better than paracetamol. They include ibuprofen which you can buy at pharmacies or get on prescription. Other types such as diclofenac or naproxen need a prescription. Some people with asthma, high blood pressure, kidney failure, or heart failure may not be able to take anti-inflammatories.
- A stronger painkiller such as codeine is an option if anti-inflammatories do not suit or do not work well. Codeine is often taken in addition to paracetamol. Constipation is a common side-effect from codeine. This may make back pain worse if you need to strain to go to the toilet. To prevent constipation, have lots to drink and eat foods with plenty of fibre.
- A muscle relaxant such as diazepam is sometimes prescribed for a few days if the back muscles become very tense and make the pain worse.
Physical treatments
Some people visit a physiotherapist, chiropractor, or osteopath for manipulation and/or other physical treatments. It is debatable
whether physical treatments would help all people with a prolapsed disc. However, physical treatments provide some short-term comfort and hasten recovery in some cases.
Surgery
Surgery may be an option in some cases. As a rule, surgery may be considered if the symptoms have not settled after about six weeks
or so. This is the minority of cases as in about 9 in 10 cases, the symptoms have eased off and are not bad enough to warrant surgery within about six weeks.
The aim of surgery is to cut out the prolapsed part of the disc. This often eases symptoms. However, it does not work in every case. Also, as with all operations, there is a risk from surgery. A
specialist will advise on the pros and cons of surgery, and the different techniques that are available.
Can further bouts of back pain and/or prolapsed disc be prevented?
Evidence suggests that the best way to prevent bouts of back pain and prolapsed disc is simply to keep active, and to exercise regularly. This means general fitness exercise such as walking, running,
swimming etc. There is no firm evidence to say that any particular 'back strengthening' exercises are more useful than simply keeping fit and active. It is also sensible to be 'back aware'. For
example, do not lift objects when you are in an awkward twisting posture.
Further information and advice
Backcare (The National Back Pain Association)
16 Elmtree Road, Teddington, Middlesex, TW11 8ST
Tel: 0870 950 0275 Web: www.backcare.org.uk
The Back Book
A reliable source of information. It is written by a team consisting of a GP, orthopaedic surgeon, physiotherapist, osteopath, and
psychologist and provides comprehensive advice. Roland, M.O et al. (2002) The back book. London: The Stationary Office.
(For reference, the above information was taken from: < httt/:www.patient.co.uk/showdoc/20700885/> )
THE ANATOMY & BASIC STRUCTURE OF THE BACK
Spinal anatomy is a remarkable combination of strong bones, flexible ligaments and tendons, large muscles and highly sensitive nerves. It is designed to be incredibly strong, protecting the highly
sensitive nerve roots, yet highly flexible, providing for mobility on many different planes. Most of us take this juxtaposition of strength, structure and flexibility for granted in our everyday
lives—until something goes wrong. Once we're in pain, we're driven to know what's wrong and what it will take to relieve the pain and prevent a recurrence.
Spinal Column
The spinal column is the centrepiece, it supports the upper body’s weight, and houses and protects the spinal cord. Stacked on top of one another are more than 30 bones (the vertebrae) that form the spinal column or spine. Each of these bones contains a roundish hole
that, when stacked in register with the others, creates a channel that surrounds the spinal cord.
Spinal Cord
The spinal cord descends from the base of the brain to just below the rib cage. Small nerves (roots) enter and emerge from the spinal cord through spaces between the vertebrae.
Cauda Equina
Because the bones of the spinal column continue growing after the spinal cord reaches its full length in early childhood, the nerve roots to the lower back and legs extend many inches down the spinal
column before exiting. This bundle of nerve roots is known as the cauda equina, or the
"horse’s tail".
Other Structures Of The Back
Spaces between the vertebrae contain round, spongy pads of cartilage called intervertebral discs that allow for flexibility in the lower back. Bands of tissue known as ligaments and tendons hold the vertebrae in place and attach the
muscles to the spinal column.
Four Regions
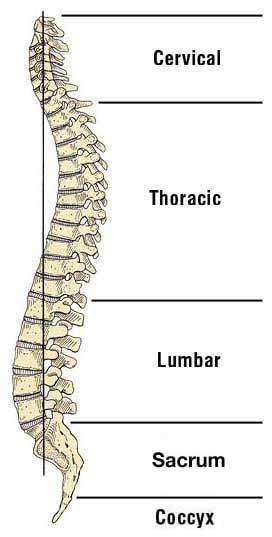
Starting at the top, the spine has 4 regions:
7 cervical (neck) vertebrae
12 thoracic (upper back) vertebrae
5 lumbar vertebrae
the sacrum and
coccyx (tailbone)
The lumbar region of the back, where most back pain is felt, supports the weight of the upper body. Many different structures in the spine are capable of producing back pain or neck pain, including:
The large nerve roots that go to the legs and arms may be irritated
The smaller nerves that innervate the spine may be irritated
The large paired back muscles (erector spinae) may be strained
The bones, ligaments or joints themselves may be injured
The disc space itself can be a source of pain
The are four major regions of the spine
The cervical spine (neck)
The neck supports the weight of the head and protects the nerves that come from the brain to the rest of the body. This section of the spine has seven vertebral bodies (bones) that get smaller as
they get closer to the base of the skull. Most of the rotation of the cervical
spine comes from the top two segments whereas most of the flexion/extension movement comes from C5-C6 and C6-C7 (each motion segment is named by the two
vertebral bodies that are connected).
Acute neck pain is most often caused by a muscle, ligament or tendon strain (such as from a sudden force or straining the neck), and will usually heal with time and conservative treatments to
alleviate the pain (such as ice and/or heat, medications, chiropractic or osteopathic manipulation, etc).
For patients with neck pain that lasts longer than two weeks to three months, or with mainly arm pain, numbness or tingling, there is often a specific anatomic problem. For example, pain that
radiates down the arm, and possibly into the hands and fingers, is usually caused by a cervical herniated disc or foraminal stenosis pinching a nerve in the neck. Treatment options for neck pain will
differ depending on the specific diagnosis.
The thoracic spine (upper back)
The 12 vertebral bodies in the upper back make up the thoracic spine.The firm attachment of the rib cage at each level of the thoracic spine provides stability and structural support to the upper
back and allows very little motion. The thoracic spine is basically a strong cage and it is designed to protect the vital organs of the heart and lungs. The upper back is not designed for motion, and
subsequently, injuries to the thoracic spine are rare.However, irritation of the large back and shoulder muscles or joint dysfunction in the upper back can be very painful.
The lumbar spine (lower back)
The lower back has a lot more motion than the thoracic spine and also carries all the weight of the torso, making it the most frequently injured area of the spine.
The motion in the lower back is divided between five motion segments, although a disproportionate amount of the motion is in the lower segments (L3-L4 and L4-L5). Consequently, these two segments are
the most likely to breakdown from wear and tear (e.g. Osteoarthritis). The two lowest discs (L4-L5 and L5-S1) take the most strain and are the most likely to herniate. This can cause pain and
possibly numbness that radiates through the leg and down to the foot (sciatica).
The vast majority of episodes of lower back pain are caused by muscle strain.Even though this doesn't sound like a serious injury, trauma to the muscles and other soft tissues (ligaments, tendons) in
the lower back can cause severe and debilitating pain. The good news is that soft tissues have a good blood supply, which brings nutrients to the injured area and facilitates the healing
process.
The sacral region (bottom of the spine)
Below the lumbar spine is a bone called the sacrum, which makes up the back part of the pelvis. This bone is shaped like a triangle that fits between the two halves of the pelvis, connecting the
spine to the lower half of the body.
The sacrum is connected to part of the pelvis (the iliac bones) by the sacroiliac joints.Pain here is often called sacroiliac joint dysfunction, and is more common in women than men.The coccyx—or the
tailbone—is in the sacral region at the very bottom of the spine. Pain here is called Coccydynia and is more common in women than men.
ANATOMICAL STRUCTURES IN THE SPINE
THE VERTEBRAE: in the cervical, thoracic and lumbar spine
Collectively, the vertebral bodies comprise the boney building blocks of the spine. They are stacked on top of each other with a disc in between each one. All of the vertebral bodies act as a support
column to hold up the spine. This column supports about half of the weight of the body, with the other half supported by the muscles.
Each area of the spine has some differences in the form and function of vertebral bodies and how they are attached to adjacent structures.
The CERVICAL SPINE has seven vertebral bodies (segments). The top two segments are unique:
The first cervical segment (called the atlas) is a ring that does not have a vertebral body. It is attached to the second vertebral body (the axis), which acts as a post that the first vertebral ring
rotates around. Most of the rotation in the neck is located in these top two segments.
Like the rest of the spine, the next five vertebral segments have three joints at each segment, including one disc in the front and paired facet joints in the back.
Unlike the rest of the spine, the segments in the cervical spine contain openings in each vertebral body for arteries to carry blood to the brain (vertebral artery running through the transverse
foramen).
The THORACIC SPINE has twelve vertebral bodies. These structures have very little motion because they are firmly attached to the ribs and sternum (breastbone). Because there is little motion, this
region of the spine is not usually a source of back pain, although the junction between the spine and the ribs (costovertebral junction) can be a source of pain.
The LUMBSR SPINE has five vertebral bodies that extend from the lower thoracic spine (upper back) to the sacrum (bottom of the spine). The vertebral bodies of the lower back are the largest of the
spine because they bear the majority of the body’s weight. The paired facet joints on the back of the vertebral segments are aligned so that they allow flexion/extension but not a lot of
rotation.
The Vertebral Body
The thick oval segment of bone forming the front of the vertebral segment is the vertebral body.
Each segment of the lumbar spine is comprised of the following structures:
The vertebral bodies are attached to a bony arch through which all the nerve roots run. The vertebral arch is comprised of two pedicles, the short stout processes that extend from the sides of the
vertebral body and two laminae, the broad flat plates that project from the pedicles and join in a triangle to form a hollow archway (the foramen).
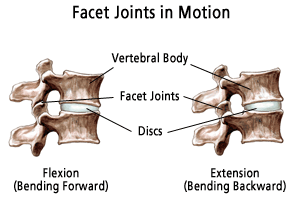
The vertebral arches are interconnected by paired facet joints, which in combination with the disc, create a three joint complex at each vertebral motion segment. This three-joint complex at each
vertebral segment (the facet joint) allows for motion in flexion, extension, rotation, and lateral bending.
The facet joints have cartilage on each surface and a capsule around them. The cartilage can degenerate as one ages, and lead to degenerative arthritis.
The spinous process protrudes from the junction of the two laminae and these are the ridges that can be felt through the skin along the back of the spine.
Transverse processes project from the junction of the pedicles and lamina. The structures of the vertebral arch protect the spinal nerves that run through the spinal canal. A lumbar laminectomy
surgery involves the removal of the laminae to gain access to the vertebral canal.
Motion in the Lower Back
Fifty percent of flexion (bending forward) occurs at the hips, and fifty percent occurs at the lower spine (lower back). The motion is divided between the five motion segments in the lower back,
although a disproportionate amount of the motion is at L4-L5 (lumbar segment 4 and 5) and L3-L4 (lumbar segment 3 and 4). Consequently, these two segments of the lower back are the most likely to
break down with degeneration. As these segments break down they can become unstable with an excess of motion creating low back pain. There are a number of non-surgical treatments available to help
manage the low back pain, and a surgical fusion can help alleviate the pain by stopping the motion.
Compression Fractures in the Vertebral Body
Since they are major load bearing structures, vertebral bodies are also prone to developing compression fractures, particularly in patients with osteoporosis (which weakens the bone). These fractures
can lead to chronic pain and progressive misalignment or deformity of the spine. Over time, a misalignment or deformity in the spine places stress on muscles, tendons, ligaments, and bones throughout
the back and can result in impaired balance or walking ability.
References:
Spinal Anatomy and Back Pain by Dr.Peter F. Ullrich, Jr., M.D.: http://www.spine-health.com/conditions/pain/spinal-anatomy-and-back-pain)
Back Pain: Discussion Paper: http://www.wsiat.on.ca/english/wsiatDocs/mlo/back_screen.htm
HUMAN TYPES
WHAT CAUSES LOWER BACK PAIN
Aging Process
As people age, bone strength and muscle elasticity and tone tend to decrease. The discs begin to lose fluid and flexibility, which decreases their ability to cushion the vertebrae.
Injury & Trauma
Pain can occur when, for example, someone lifts something too heavy or overstretches, causing a sprain, strain, or spasm
in one of the muscles or ligaments in the back.
If the spine becomes overly strained or compressed, a disc may rupture or bulge outward. This rupture may put pressure on one of the more than 50 nerves rooted to the spinal cord that control body
movements and transmit signals from the body to the brain. When these nerve roots become compressed or irritated, back pain results.
Low back pain may also reflect:
nerve irritation
muscle problems
bone lesions
Other Causes: Most low back pain follows injury or trauma to the back, but pain may also be caused by:
osteoarthritis
osteoporosis or other bone diseases
viral infections
irritation to joints and discs
congenital abnormalities in the spine
scar tissue
Other factors that contribute to low back pain include:
obesity/weight gain
smoking
stress
poor physical condition/posture
poor sleeping position
Serious Problems
Low back pain may also indicate a more serious medical problem. People with back pain along with fever, loss of bowel or bladder control, pain when coughing, progressive weakness or pain radiating
into the legs should contact a doctor immediately to help prevent permanent damage.Ref: What Causes Lower Back Pain:
http://arthritis.about.com/od/backpain/ss/lowbackpain_3.htm
- TYPES OF BACK PAIN
- HOW TO DEAL WITH BACK PAIN - TRADITIONAL AND MODERN APPROACHES
- PHYSIOTHERAPY AND EXERCISES
- BASIC PAIN RELIEF